Cerebral Palsy When and How to Address Surgically with Early and “Tailor-made” surgery
Cerebral Palsy When and How to address surgically with early and “tailor-made” surgery
As we have already pointed out several times, patients with cerebral palsy (CP) should be treated with a multidisciplinary approach, involving all specialists (neurologists, physiotherapists, gastroenterologists and even dentists) who can offer their contribution, both from a diagnostic and therapeutic point of view, to improve the clinical and living conditions of these subjects.
It is essential to address children with a 360-degree approach.
Of course, orthopaedics, or rather neuro-orthopaedics, also play a very important role in this process.
Patients with CP need to undergo orthopaedic surgery more than once in their lifetime. For this reason, defining the optimal timing and modalities of orthopaedic surgery is a key step in achieving better results and avoid unnecessary extra surgery. This is also important from a psychological point of view for the patient and his/her family.
THE STEPS
Clinical evaluation
The orthopaedic surgeon and his team should carry out a combined clinical evaluation of the patient to gather as much information as possible and to quantify the various movement and/or gait defects.
Recently, specialists have adopted a functional approach to analyze and observe some clinical features such as:
- Strength
- Resistance
- Esauribilty
- Motor coordination
- Balance and proprioception
- Spasticity
- Range of motion
This is a very different approach from the past, when only the lack of joint motion was evaluated, for example. The evaluation of patients affected by Cerebral Palsy must be functional and not only anatomical and is based on the Gross Motor Function Classification System (GMFCS) which is divided into five levels summarized as follows:
| GMFCS Level I | Children walk at home, outdoors and in the community. They can climb stairs without the use of a railing. Children perform gross motor skills such as running and jumping, but speed, balance and coordination are limited. |
| GMFCS Level II | Children walk in most settings, indoor and outdoor and climb stairs holding onto a railing. They may experience difficulty walking long distances and balancing on uneven terrain, inclines, in crowded areas or confined spaces. |
| GMFCS Level III | Children walk using a hand-held mobility device in most indoor and outdoor settings. They may climb stairs holding onto a railing with supervision or assistance. Children use wheeled mobility when traveling long distances and may self-propel for shorter distances. |
| GMFCS Level IV | Children may walk for short distances at home with physical assistance or use powered mobility or a body support walker when positioned. At school, outdoors and in the community children are transported in a manual wheelchair or use powered mobility. |
| GMFCS Level V | Children are transported in a manual wheelchair in all settings. Children are limited in their ability to maintain antigravity head and trunk postures and control leg and arm movements. |
Thanks to these initial evaluations, the orthopaedic surgeon may already have an idea of the type of treatment to be adopted and the achievable goals, which may be:
- Avoiding the progression of the disease (GMFCS 1→5)
- Restore the 5 requirements for normal walking (GMFCS 1→3)
- Eliminate any algic symptoms caused by skeletal deformities (hips/knees/foot) (GMFCS 1→5)
Diagnostic examinations
Of course, before proceeding, the orthopaedic surgeon must provide a series of evaluations for a proper study of the musculoskeletal system, such as for example:
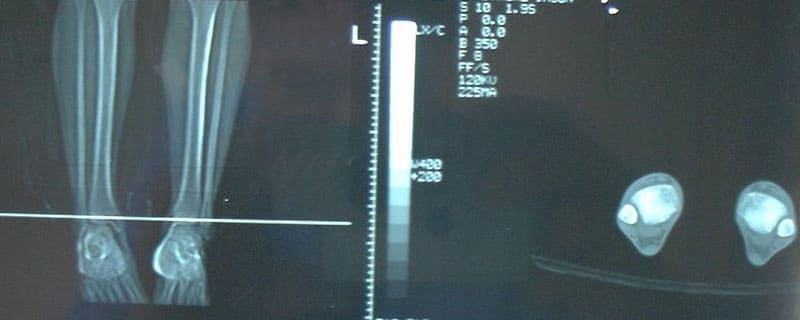
- X-ray of the pelvis
- Standing long film x-ray of the lower limbs
- The study of torsional profiles (with CT Scan)
- Gait analysis (GA)
- Dynamic surface electromyography (EMG)
All these evaluations offer an overview of the biomechanical pathological changes and allow to evaluate if and how to proceed with surgery.
The main goal will be to obtain an improvement in child gait.
Thanks to this new approach, it is possible not only to correct the most obvious defects, as in the past, but it is also possible to intervene on the compensations associated with them.
In addition to this, thanks to the study of the molecular behaviour of the tendons (Portinaro et al. ) it is also possible to define, in an optimal way, the exact timing of surgery.
In general, it is preferable to perform early surgery, especially on the bony section, before the tendons undergo degeneration due to the pathological stimulus of spasticity.
Timing and tailoring become the key word for surgery.
Surgery
Surgery is, therefore, the final act of a series of complex evaluations of the patient and his/her specific patterns. We can, therefore, talk about a tailor-made treatment.
Surgery can be:
- early and preventive
- late and corrective
This depends on the age of the patient and the severity of the deformity he/she is affected.
In this blog, we will deal with the first case: early and preventive surgery.
At our center we have developed an algorithm, which has been scientifically and clinically validated in the last 10 years, that has allowed us to make an early and minimally invasive surgery to prevent and correct major bone deformities, the so called Lever Arm Disease (LAD).
The advantage of early surgery is to exploit the growth potential of bones in order to correct the various deformities in a biological way. For example thanks to temporary epiphysiodesis we can control asymmetrically the growth plates of the bones.
All these procedures can be used, for example, in the proximal femur, the distal femur, the proximal tibia and the foot.
Wherever possible, it is, therefore, preferable to proceed with early treatment and minimally invasive surgery.
Nowadays children can undergo surgery at the age of 5 or 6 years and thanks to this approach it is also possible to optimize the results and recovery times after the operation.
Not to mention that these operations are usually outpatient procedures.
It is therefore advisable for patients with Cerebral palsy to undergo orthopaedic and multidisciplinary evaluations as soon as possible in order to intervene when the growth potential is greater.
Also, small patients can benefit from a higher speed of functional recovery, which can start already in the first postoperative day.
Of course, this also allows for faster healing.
In the next blog, we will focus on late surgery for Cerebral Palsy, i.e. what can be done when patients have reached, or almost reached, the end of their growth.